Surface Barriers
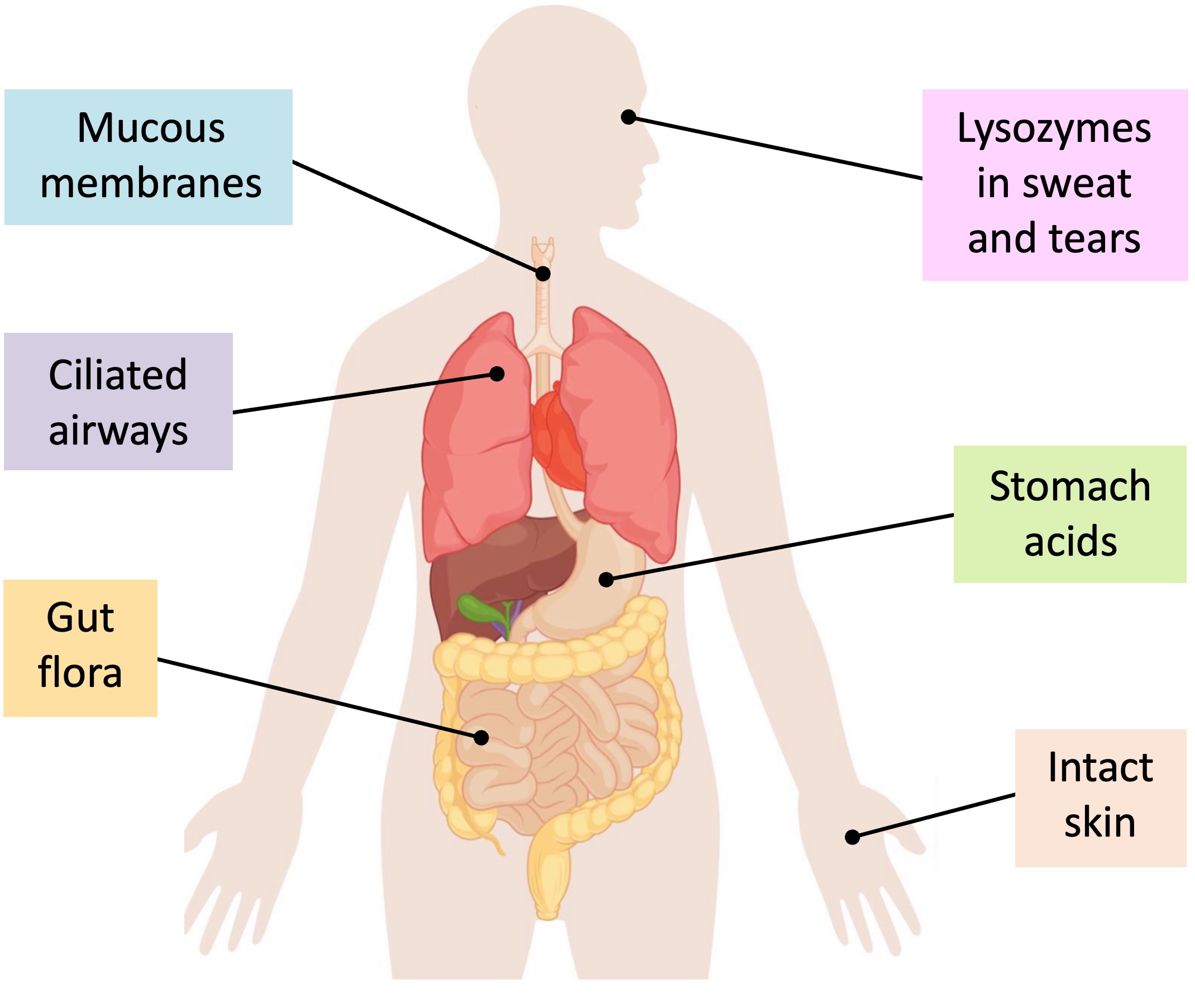
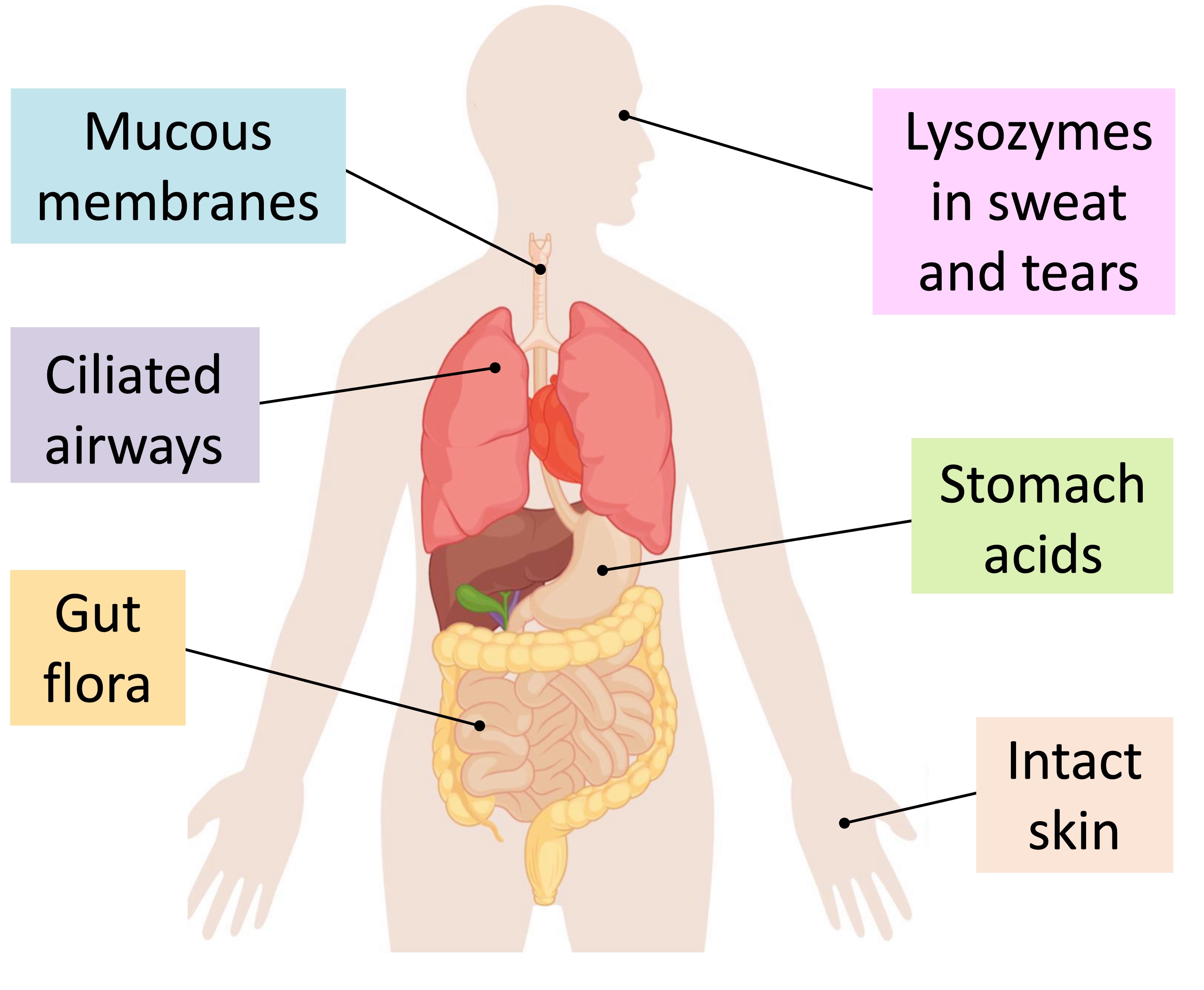
The first line of defence against infectious disease are the surface barriers that prevent the entry of pathogens into the body
-
These barriers can include physical, chemical and microbiological impediments
Physical Barriers
-
Skin covers external surfaces and consists of a layer of dead cells that provides protection when intact
-
Mucous membranes line internal surfaces (e.g. cavities and tubes) and consist of a thin layer of living cells that secrete mucus
-
Mucous membranes may be ciliated (e.g. airways) to assist in the trapping and subsequent removal of pathogens
-
Chemical Barriers
-
Exocrine glands connecting to the skin (e.g. sebaceous glands) or internal cavities (e.g. gastic glands) may release antimicrobial agents
-
Sebaceous glands secrete chemicals (such as lactic acid) that inhibit microbial growth on the surface of the skin
-
Tears and saliva contain lysozyme (enzyme) which can destroy cell walls, while sticky mucins (in mucus) help to clear pathogens
The stomach and genitourinary tracts both produce acids in order to create a hostile pH range to pathogens in these regions
-
Microbiological Barriers
-
Microbiotic barriers consist of the normal flora (commensals) that line specific cavities (such as the digestive tract) in most animals
-
By occupying the available space in the intestines, the microbiota prevents the colonisation of these surfaces by pathogenic cells
-
Surface Barriers
Clotting
Blood clotting is the mechanism by which broken blood vessels are repaired when damaged
-
Clotting functions to limit pathogenic access to the bloodstream when the skin is broken (and also prevent excess blood loss)
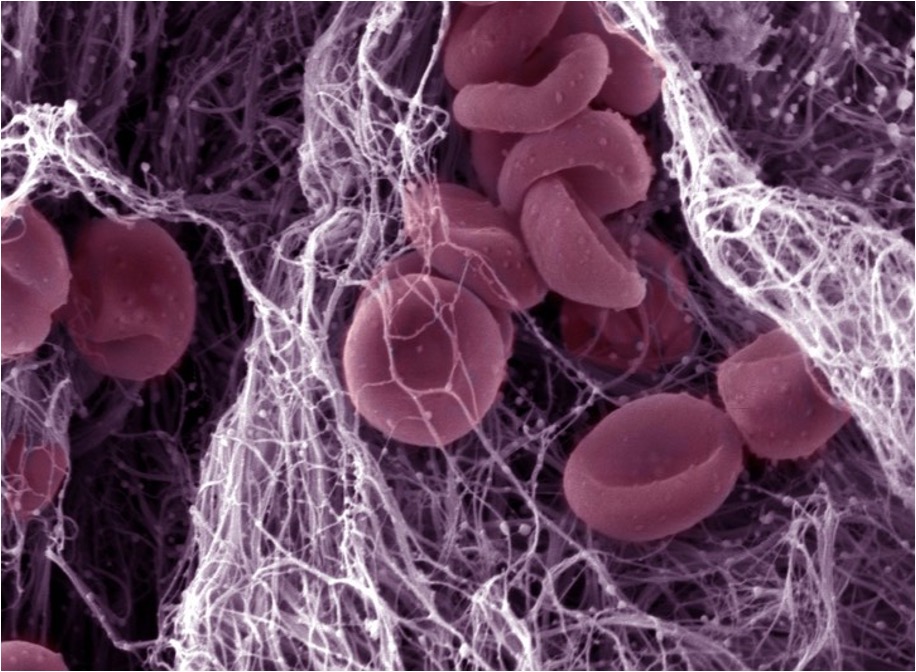
There are two key components of a blood clot – platelets and insoluble fibrin strands
-
Platelets undergo a structural change when activated to form a sticky plug at the damaged region
-
Fibrin strands form an insoluble mesh of fibres that trap blood cells at the site of damage
Coagulation Cascade
The process by which blood clots are formed involves a complex set of reactions collectively called the coagulation cascade
-
Damaged cells release clotting factors, which cause platelets to become sticky and form a solid plug at the damaged region
-
Clotting factors also trigger the conversion of the inactive zymogen prothrombin into the activated enzyme thrombin
-
Thrombin in turn catalyses the conversion of the soluble plasma protein fibrinogen into an insolube fibrous form called fibrin
-
The fibrin strands form a mesh of fibres around the platelet plug and traps blood cells to form a temporary clot
-
When the damaged region is completely repaired, an enzyme (plasmin) is activated to dissolve the clot
Clotting Components
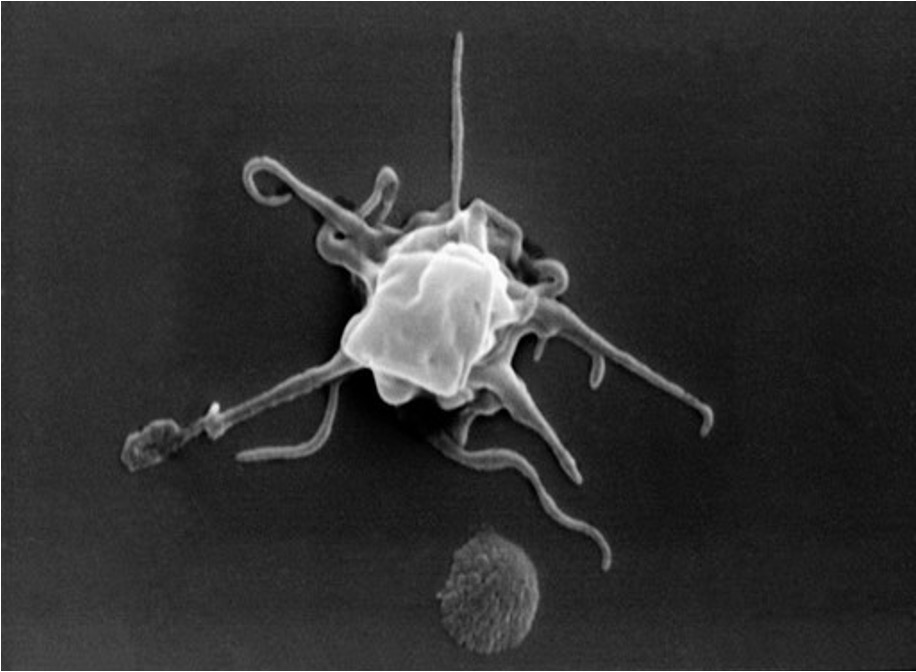
Activated platelet