

Menstrual Cycle
The menstrual cycle describes recurring changes that occur within the female reproductive system to make pregnancy possible
-
Each menstrual cycle lasts roughly one month (~28 days) and begins at puberty (menarche) before ending with menopause
There are two key groups of hormones which control and coordinate the menstrual cycle:
-
Pituitary hormones (FSH and LH) are released from the anterior pituitary gland and act on the ovaries to develop follicles (ovarian cycle)
-
Ovarian hormones (estrogen and progesterone) are released from the ovaries and act on the uterus to prepare for pregnancy (uterine cycle)
Stages of the Menstrual Cycle
There are two key stages to the menstrual cycle that are controlled by changes to hormone levels
-
The ovarian cycle constitutes the development of follicles within the ovaries and the subsequent release (via ovulation) of an oocyte
-
The uterine cycle constitutes the development of the endometrial lining within the uterus and its eventual shedding (via menstruation)
1. Ovarian Cycle
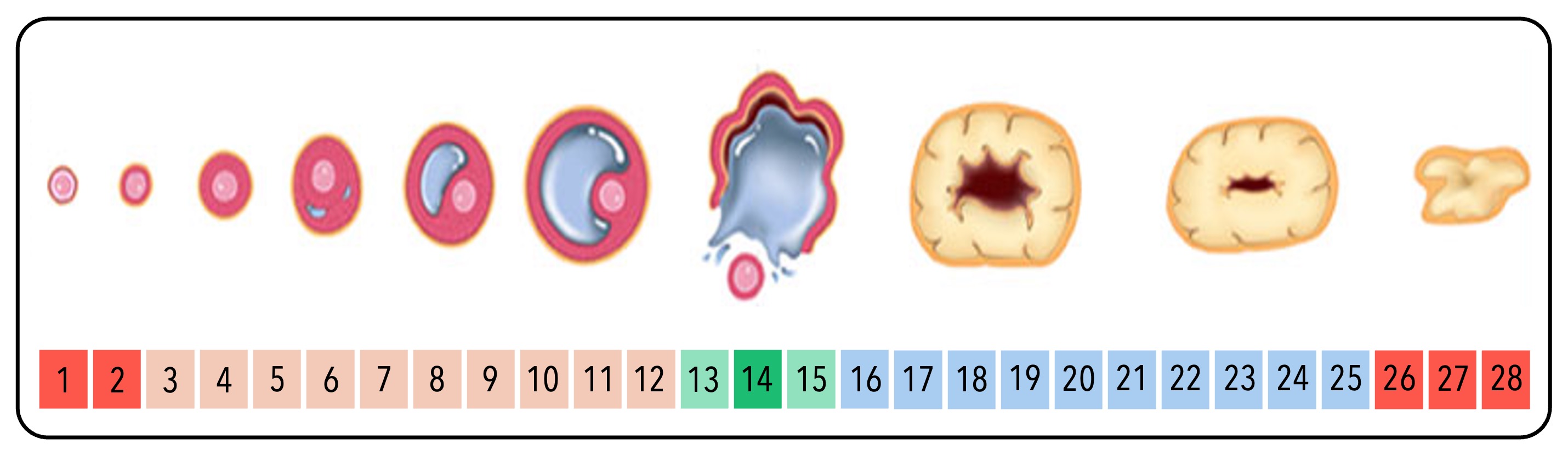
The ovary contains many immature eggs within undeveloped primordial follicles
-
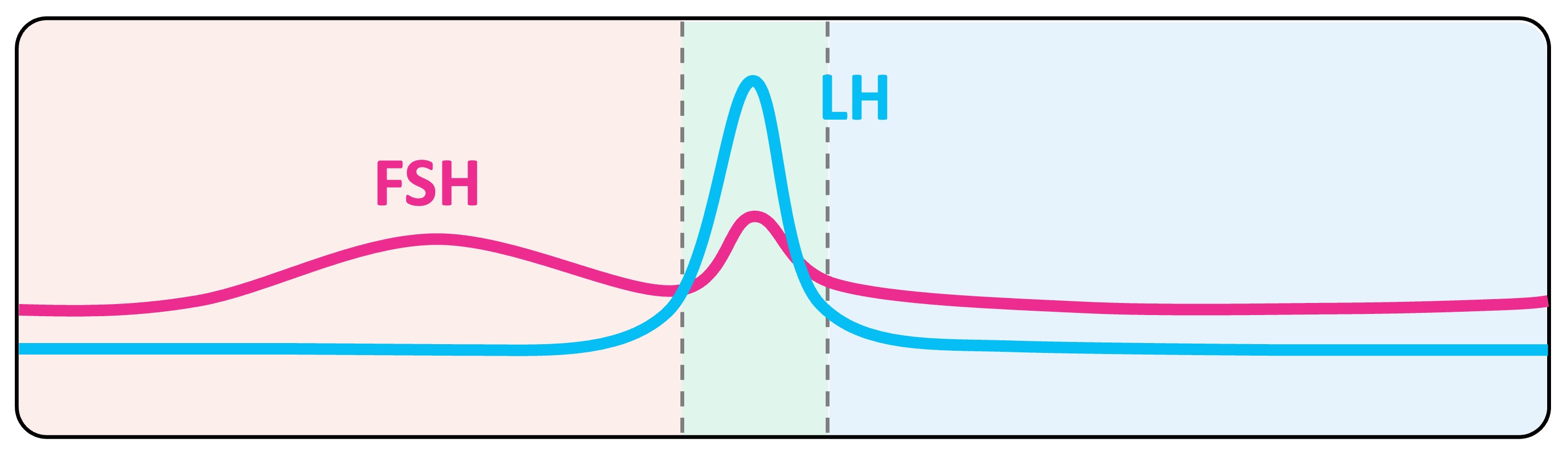
At the beginning of the cycle, follicle stimulating hormone (FSH) is secreted from the anterior pituitary and stimulates growth of ovarian follicles
-
The dominant follicle produces estrogen, which inhibits FSH secretion via negative feedback to prevent other follicles growing
-
Midway through the cycle (~ day 12), estrogen concentrations reach a critical threshold which stimulates the anterior pituitary to release hormones via positive feedback
-
This positive feedback results in a large surge of luteinizing hormone (LH) and a lesser surge of FSH
-
LH causes the dominant follicle to rupture and release an egg (secondary oocyte) – this is called ovulation
-
The ruptured follicle develops into a corpus luteum that secretes high levels of progesterone, as well as lower levels of estrogen
-
Estrogen and progesterone inhibit the further secretion of FSH and LH, preventing other follicles from developing while the corpus luteum is active
-
However, the absence of FSH also prevents the corpus luteum from being maintained, resulting in its gradual degeneration
-
When the corpus luteum is fully degenerated, estrogen and progesterone levels drop and FSH levels will rise – beginning the cycle anew
Pituitary Hormone Levels
Follicle Development
2. Uterine Cycle
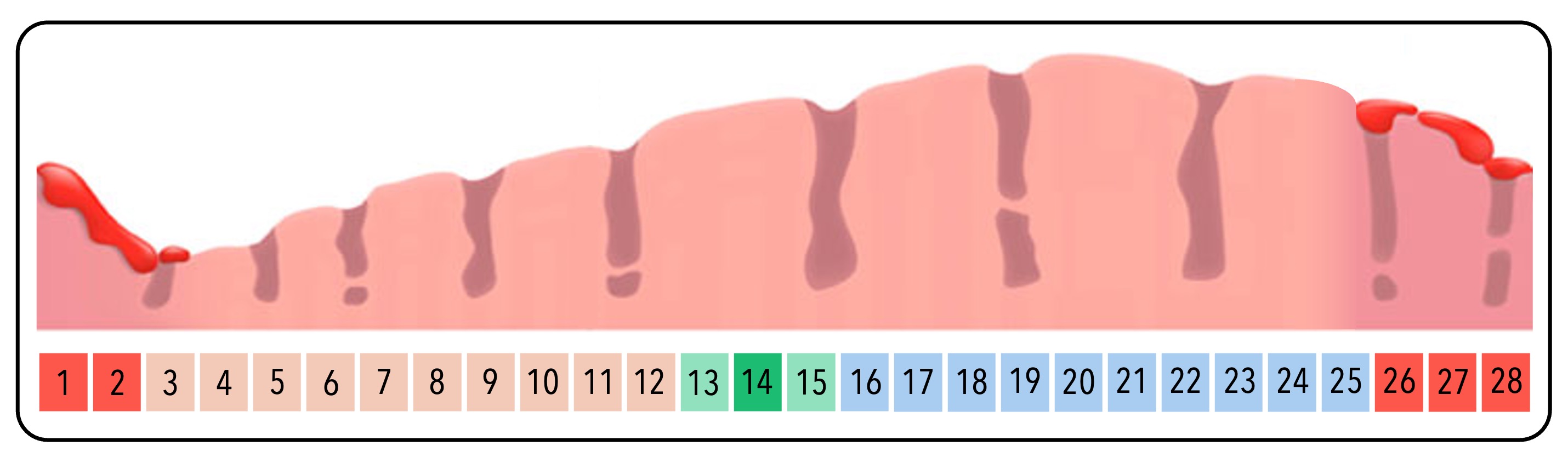
The endometrial lining of the uterus functions as the location where a fertilised egg will develop
-
At the beginning of the cycle, the FSH released from the pituitary gland stimulates the production of estrogen by the ovarian follicles
-
This estrogen acts on the uterus to stimulate the thickening of the endometrial layer
-
Midway through the cycle, the follicle ruptures (ovulation), resulting in a brief dip in estrogen levels
-
The corpus luteum that develops will produce both progesterone and estrogen, causing these hormone levels to progressively rise
-
These hormones act to further support the thickening and maintenance of the endometrial lining while the oocyte is in transit
-
If the corpus luteum degenerates, estrogen and progesterone levels fall, meaning the endometrium can no longer be maintained
-
The endometrial layer is sloughed away and eliminated from the body as menstrual blood (i.e. a period) – the cycle can now begin anew
Ovarian Hormone Levels

Endometrial Lining
In the event of pregnancy:
The endometrial lining of the uterus functions as the location where a fertilised egg will develop
-
If a released oocyte is fertilised by a sperm, the developing embryo will implant in the endometrium and release hormones to sustain the corpus luteum
-
This will prevent estrogen and progesterone levels from dropping, meaning the endometrium is not sloughed away (no menstruation while pregnant)
-
The corpus luteum will be maintained until a specialised organ called the placenta is formed – it then releases the progesterone needed to sustain the endometrial layer (and the estrogen needed to prevent folliclular development)




